Discoloured semen: Signs, Symptoms, and When to Seek Help?
6562
Discoloured semen indicate health issues. Normal is white/clear; yellow or green suggests infection, while red or black may signal serious conditions.
What Causes Changes in Semen Colour, and What Do They Indicate?
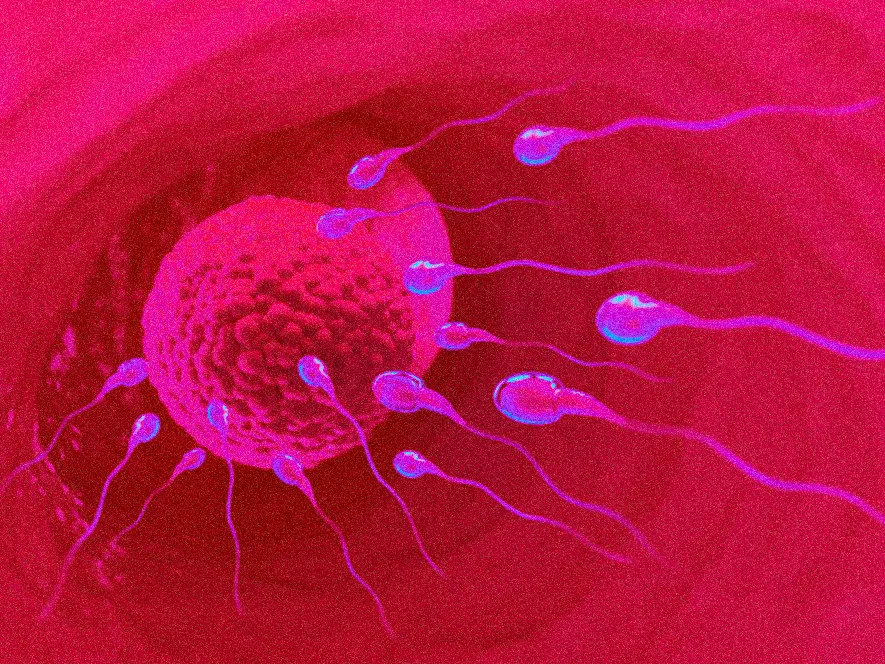
Semen colour, texture, and even smell may vary slightly and still be considered normal. However, significant changes in semen colour could indicate potential health issues, such as the presence of blood or infections.
Healthy semen typically appears as a cloudy white with a jelly-like consistency. A gradual yellowing may occur due to ageing or prolonged abstinence, which usually isn't a concern. On the other hand, other colour changes in semen can suggest an underlying health problem or physical complication.
Book Your Appointment Today!
Contact us at info.bkk@pulse-clinic.com or chat on your preferred platform:
![]() +66 65 237 1936
+66 65 237 1936  @PULSEClinic
@PULSEClinic ![]() PulseClinic
PulseClinic
Discoloured Semen: What Does It Mean?
Discolouration of semen can be a concern and may indicate underlying health issues. Here’s a breakdown of common semen colours and their potential meanings:
- White or Clear: This is considered normal and indicates healthy semen.
- Yellow: This can result from dehydration or may indicate an infection, such as a urinary tract infection (UTI) or sexually transmitted infection (STI).
- Green: Green semen may also suggest an infection, particularly a sexually transmitted infection. It is important to consult a healthcare provider if this occurs.
- Red or brown: This usually indicates the presence of blood in the semen, known as hematospermia. This can result from various conditions, including infections, inflammation, or injury to the reproductive organs.
- Black: Black semen is rare and may signify a serious condition, such as old blood from a previous injury or an underlying health problem. Immediate medical evaluation is recommended.

Should I Be Worried About Discoloured Semen?
Semen typically has a whitish-grey appearance. Changes in its colour may be temporary and harmless, but they can also indicate an underlying issue that warrants further investigation.
Here are possible causes based on colour:
- Red Semen: This may result from inflammation in the prostate or the glands responsible for semen production. While it can be concerning, especially for younger men, the underlying cause is often benign.
- Yellow or Green Semen: These colours may indicate an infection, jaundice, or the influence of vitamins or medications.
If you notice a change in semen colour that persists for more than a week, it’s important to consult your doctor or see a urologist for a proper evaluation.
Why does semen colour change?
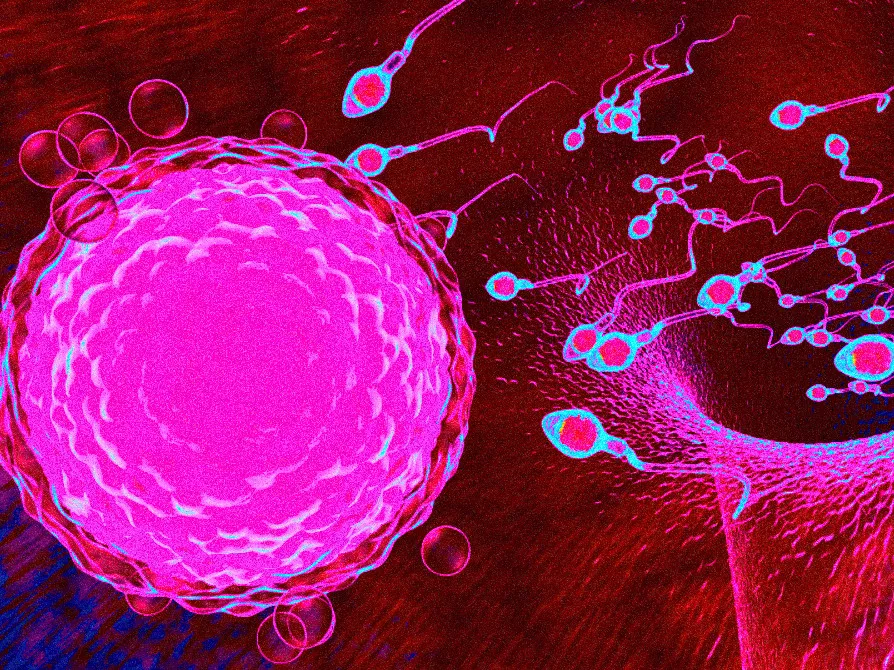
Understanding Semen and Its Composition: Semen plays a crucial role in the male reproductive system. While it primarily consists of sperm, it is also a complex fluid that includes various other substances, such as:
- Vitamins
- Enzymes
- Minerals
- Proteins
- Antioxidants
- Sugars
Healthy semen typically appears as a cloudy white or grey liquid, resembling raw egg whites or runny jelly in consistency. Additionally, it has an alkaline odour similar to that of bleach.
Add us on Line and stay in touch.
Understanding Changes in Semen Colour and Their Implications
If semen appears pink or reddish brown, it may indicate the presence of blood, a condition known as hematospermia. There are several potential causes for bloody semen, including:
- Sexually transmitted infections
- Prostate biopsy
- Enlarged prostate (benign prostatic hyperplasia, BPH)
- Prostatitis (inflammation of the prostate)
- Brachytherapy (a type of radiation treatment for prostate cancer)
- Epididymitis (inflammation of the epididymis, the tube that stores sperm)
- Urethritis (inflammation of the urethra)
- Injury or trauma
- Vasectomy
In rare instances, hematospermia may also be linked to testicular cancer or prostate cancer. However, most often, no specific cause can be identified, and the presence of blood in semen is benign.
Yellow semen may be associated with conditions such as:
- Sexually transmitted infections
- Leukocytospermia (elevated white blood cell count)
- Urine mixing with semen, particularly if there has been a delay in ejaculation
- Jaundice
- Dietary changes, including consumption of foods with dyes
Green semen may suggest a sexually transmitted infection or prostatitis.
Treatment for changes in semen colour depends on the underlying cause. For instance, men diagnosed with prostatitis or a sexually transmitted infection may require antibiotics.
Men are typically attuned to their bodies and can often recognise the normal colour of their semen. However, if there are any noticeable changes in colour, consistency, or if a foul odour is detected, it's wise to consult a doctor. Additionally, symptoms such as pain, burning sensations, swelling, itching, or any other unusual signs should be addressed promptly with a healthcare professional.
What Different Textures of Semen May Indicate
In addition to colour changes, variations in semen texture can also cause concern for some individuals. These textural alterations can be influenced by several factors.
Healthy semen can naturally exhibit different textures, appearing either slightly thicker or more watery based on:
- Diet
- Lifestyle choices, including physical activity levels
- Alcohol consumption
- Drug use
Typically, a temporary change in semen texture is not a cause for alarm. Even minor factors, such as temporary dehydration, can result in thicker semen for a brief period.
However, if texture changes occur alongside other issues, such as an unpleasant odour or alterations in colour, it may be advisable to consult a healthcare professional.
When to Consult a Doctor
While some changes in semen colour may not warrant concern and often do not require medical intervention, persistent alterations accompanied by additional symptoms—such as an unpleasant odour or prolonged hematospermia—should prompt a consultation with a healthcare provider.
Individuals experiencing signs of potential prostate issues should also seek medical advice. Symptoms to watch for include difficulty urinating, swelling in the genital or pelvic areas, pressure in the colon, or a persistent urge to have a bowel movement.
Timely detection and treatment can significantly improve the chances of addressing any underlying issues effectively.
Conclusion
Healthy semen typically appears clear, white, or gray. While changes in colour may be temporary and resolve on their own, individuals should seek medical attention if these changes persist or occur alongside other symptoms, such as signs of infection or inflammation.
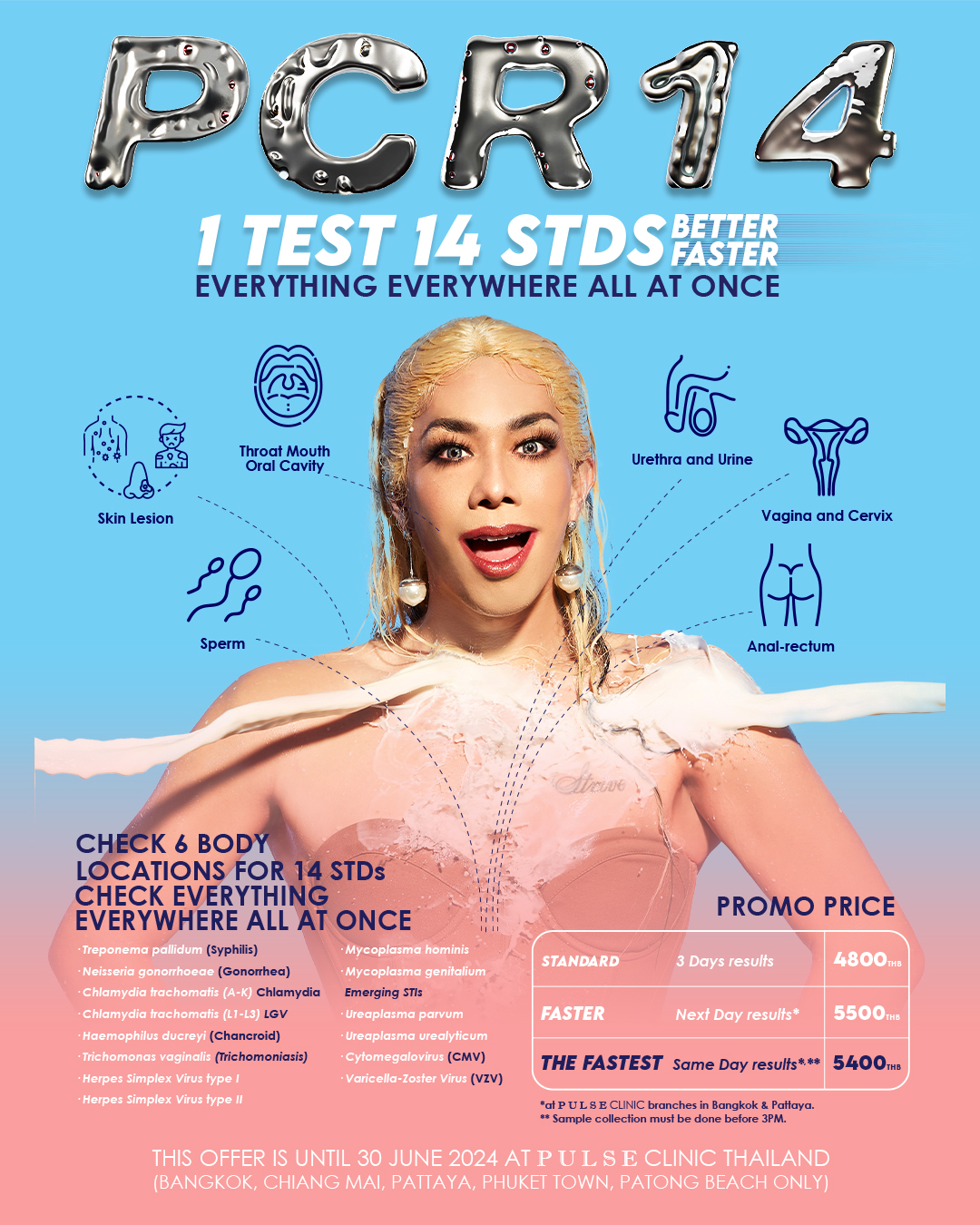
PCR 28 for Sexually Transmitted Diseases (STDs)
PCR 28 can provide comprehensive testing for 28 pathogens that can be related to STDs and other related symptoms. PCR stands for Polymerase Chain Reaction; it is also called Nucleic Acid Amplification Test (NAAT) and is a modern molecular technique used to detect a particular pathogen (virus or bacterium) in a specimen of blood, body fluid, or other tissue. This technique detects virus or bacterial DNA. The nucleic acid amplification test (NAAT) is the recommended testing method for Chlamydia, Gonorrhoea, Ureaplasma, Mycoplasma, and Trichomonas, among other infections. It has very high specificity (higher than 99.5%) and higher sensitivity and accuracy than culture (the old diagnosis technique). In both men and women, painless urine PCR (yes, you just have to pee) and genital PCR were significantly more sensitive than culture. It can detect infection, whether the organism is dead or alive! This is mostly done in first-world countries and medical schools.
All PULSE clinics in Thailand provide the most comprehensive PCR tests for 28 infections to give you peace of mind and fast treatment.
Book Your Appointment Today!
Contact us at info.bkk@pulse-clinic.com or chat on your preferred platform:
Loading...
Clinic Locations
Loading...