The Advantages of Using Multiplex PCR for the Simultaneous Detection of 14 Sexually Transmitted Diseases (Part 2) | Most advanced DNA test in Bangkok, Pattaya, Phuket, Thailand
4103
Asymptomatic testing, get tested even though you don't have any symptoms PCR Multiplex for 14 infections - Most advanced DNA test in Bangkok, Pattaya
Written by Dr.Deyn Natthakhet Yaemim (Founding Director) on 6 June 2015, Last updated 18 July 2022
The Advantages of Using Multiplex PCR for the Simultaneous Detection of Six Sexually Transmitted Diseases (Part 2)
4. Multiplex PCR methods as diagnostic tools for STDs
Multiplex PCR methods for the simultaneous diagnosis of several STDs are more and more often employed in recent years. These methods place a number of primer pairs corresponding to specific DNA sequences of various STD pathogens all in one reaction tube, such commercial ready to use kits being available. While some kits can simultaneously detect two commonly associated STDs, such as C. trachomatis and N. gonorrhoeae infections, others can manage three pathogen detections. However, kits containing the primer pairs needed for the simultaneous detection of 6–12 STD pathogens are gaining momentum on the market. The most effective and widely used kits are presently those simultaneously detecting the top six most frequent STD agents, namely C. trachomatis, N. gonorrhoeae, T. vaginalis, U. urealyticum, M. hominis and M. genitalium, agents which play hard to get for other detection methods and often exhibit multiple associations.
Another asset is that easily collectable urine samples are adequate DNA sources for these PCR techniques along with the urethral/vaginal discharge swabs. About 30–50 mL of first void urine (FVU) samples collected in sterile polypropylene containers early in the morning, at least 4 h after the previous urination, are more than enough for a successful analysis. FVU is definitely less invasive compared to the harvesting of vaginal or urethral secretions, an aspect reported to have influenced a significant number of subjects to avoid STD identification tests previously [48]. As urine specimens can be self‐collected in intimacy, an increased number of patients tend to favor such option that also enhances the applicability of the screening programs [49]. The fact that urethral secretions were found to present increased sensitivity and specificity compared to FVU in immunological analyzes for male subjects seems to hold lesser relevance, anyway differences have diminished since NAAT were first performed [46]. Concerning the female subjects, the use of urine specimens in STD identification produced similar results to vaginal or endocervical secretions [50]. It is known that assay sensitivity may decrease if samples are repeatedly frozen/thawed or stored for longer periods of time because nucleic acids can easily degrade. Urine samples hold another advantage as well: they can be stored at 4–8°C up to 7 days prior to the processing.
Thanks to this easy and noninvasive sampling, the multiplex PCR can be used to detect STDs in both symptomatic and asymptomatic individuals and could prove to be a useful screening tool for the general population.
A 15 min centrifugation at 15,000g and subsequent supernatant removal and pellet resuspension are needed as a successful DNA extraction requires concentrated pathogen suspensions. Both urethral/vaginal discharge swab specimens and urine samples should be brought to room temperature prior to the centrifugation. One can use up to 10 mL amounts of sample to increase the DNA extraction yield. Several commercially available kits for DNA extraction can be used according to the manufacturer's instructions, e.g., QIAamp® DNA Mini Kit (Qiagen, Hilden, Germany), AccuPrep Genomic DNA Extraction Kit (Bioneer, Seoul, Korea) or MasterPure™ Complete DNA and RNA Purification Kits (Epicentre Biotechnologies, USA).
In our marketing era, such new techniques and gadgets (kits) need to be accompanied by studies assessing their performance compared to other traditional methods.
One such study conducted in 2010 [36] compared the multiplex PCR assay for the simultaneous detection of T. vaginalis, U. urealyticum and M. hominis with data obtained using microscopic and culture techniques. Three cotton swabs were obtained from each of the 240 women enrolled in the study based on claims of lower genital tract infections. For the detection of T. vaginalis, swabs were inoculated in a modified Diamond's Trypticase‐yeast medium including fetal bovine serum, streptomycin, penicillin G and amphotericin B and a wet mount was prepared for its detection by direct microscopic examination. The samples were incubated at 37°C in carbon dioxide atmosphere and observed for a week under a light microscope. The presence of M. hominis and U. urealyticum was assessed by culture detection using the Mycoplasma Duo kit (Sanofi Diagnostic). A number of different primer sets were synthesized, PCR amplifications and ethidium bromide detections in 1% agarose gels were performed for a multiplex PCR to be designed for the simultaneous detection of T. vaginalis, M. hominis and U. urealyticum. Results were then favorably compared to more conventional methods for the detection of T. vaginalis, M. hominis and U. urealyticum. When tested on vaginal swabs, the multiplex PCR correctly detected 14 out of 14 T. vaginalis‐positives, 95 of 98 U. urealyticum‐positives and 22 out of 22 M. hominis‐positive samples. In contrast, the microscopic detection of T. vaginalis exhibited a 28.6% sensitivity, whereas culture methods identified 71.4% of the trichomonad infections documented with multiplex PCR. While the kit's sensitivity in the detection of U. urealyticum was 96.9%, a value comparable to culture test sensitivity (91.8%), identification of M. hominis was greatly improved (100 vs. 36.3% sensitivity). The study argued for multiplex PCR superiority in terms of sensitivity and rapidity (hours vs. days/weeks).
Another study [43] in 2011 compared the results of 113 STD patients tested for six sexually transmitted microorganisms (C. trachomatis, M. hominis, M. genitalium, N. gonorrhoeae, T. vaginalis and genital Ureoplasma) with an automated Seeplex® (Seegene, Korea) multiplex PCR‐based STD6B autocapillary electrophoresis (ACE) system vs. culture and conventional PCR‐based tests on genital and urinary specimens. C. trachomatis was cultured on cycloheximide‐treated McCoy cells, while A7, arginine broth and agar media were used for M. hominis and Ureaplasma. Conventional culture media were employed for N. gonorrhoeae.N. gonorrhoeae and C. trachomatis was also tested with the PCR‐based COBAS Amplicor. On the other hand, in‐house validated PCR assays were performed for T. vaginalis, N. gonorrhoeae and C. trachomatis, while a Hy‐Mycoplasma PCR Detection Kit (Hy‐Labs, Israel) enabled the detection of M. hominis, M. genitalium and Ureaplasma. All six pathogens (T. vaginalis, M. hominis, M. genitalium, C. trachomatis, N. gonorrhoeae and Ureaplasma) were subjected to a multiplex PCR amplification and the products were separated and detected via automated capillary gel electrophoresis. The sensitivity of the STD6B ACE kit was 100% in case of C. trachomatis, N. gonorrhoeae, M. genitalium, T. vaginalis and M. hominis, and 98% for the Ureaplasma. Specificity was also 100% for C. trachomatis, N. gonorrhoeae, M. genitalium and T. vaginalis, while for M. hominis and Ureaplasma figures were 99 and 97%, respectively. These results prove beyond any doubt that the integrated STD6B ACE system is highly effective in the detection of each of the six STD pathogens depicted from a single specimen.
Seeplex® STD6 ACE Detection kit (Seegene, Korea) was evaluated in yet another Korean study, completed in 2012, which was conducted on 739 subjects [51]. Cervical swabs were collected from the women enrolled, while men were requested to provide 30–40 mL of FVU. The six pairs of dual priming oligonucleotide primers specifically targeting the C. trachomatis, M. hominis, M. genitalium, N. gonorrhoeae, T. vaginalis and U. urealyticum genes were tested against a combined monoplex PCR. All specimens were tested with the multiplex PCR for the six pathogens and amplification products were separated with a LabChip® DX Seeplex® assay system (Caliper, USA). All specimens were retested with six monoplex PCRs (one for each of the STD agents) and a duplex strand displacement amplification (SDA) for C. trachomatis and N. gonorrhoeae was accomplished with a BD ProbeTec™ (Becton–Dickinson Microbiology System, USA). An absolute correlation between the multiplex and monoplex PCRs was found in terms of both sensitivity and specificity. The results of the multiplex PCR and duplex SDA were 99.7% concordant in the case of C. trachomatis and 100% for N. gonorrhoeae. The results confirmed that the simultaneous detection of several species in one sample was feasible and that the clinical sensitivity provided by the multiplex PCR was on an equal footing with the monoplex PCR and duplex SDA, proving to be fully adequate for routine detection of several STDs while holding an upper hand in terms of cost‐effectiveness and rapidity.
Anyplex™ II STI‐7 Detection Kit (Seegene, Korea) was tested to the limit in a 2013 Korean study [46] aiming to investigate the accuracy and reliability of a real‐time multiplex PCR assay employed for the detection of seven STD agents (C. trachomatis, N. gonorrhoeae, T. vaginalis, M. genitalium, M. hominis, U. urealyticum and U. parvum) in clinical samples. A total of 897 specimens (696 FVU and 201 endocervical swabs) were collected from 365 symptomatic patients and 532 asymptomatic volunteers and five diagnostic methods were employed as the specimens were subjected to parallel testing using four NAATs and one Mycoplasma detection kit. The RT‐PCR amplification was performed for all seven microorganisms with Anyplex™ II STI‐7 Detection Kit. PCR amplification was performed using the Seeplex® STD6 ACE Detection Kit, in accordance with the manufacturer's protocol. A battery of kits were deployed for detecting the pathogens: C. trachomatis and N. gonorrhoeae—SDA technology using BD ProbeTec™; T. vaginalis and M. genitalium—AmpliSens® (EPH PCR Kit‐InterLabService Ltd, Russia); M. hominis and U. urealyticum—Mycoplasma IST 2 Kit (bioMérieux, France). Test sensitivity and specificity of each method for every STD agent were calculated in parallel and conclusions were that the multiplex real‐time PCR (Anyplex™ II) demonstrated outstanding results compared with other diagnostic tools as it yielded 100% sensitivity and very high specificity in the detection of C. trachomatis, N. gonorrhoeae, T. vaginalis, M. genitalium and M. hominis and was also useful in discriminating between U. urealyticum and U. parvum. Despite the increased workload and higher costs due to the larger number of tests conducted, multiplex real‐time PCR was found to be equivalent or superior to other assessment methods and in the future is expected to become a standard diagnostic tool.
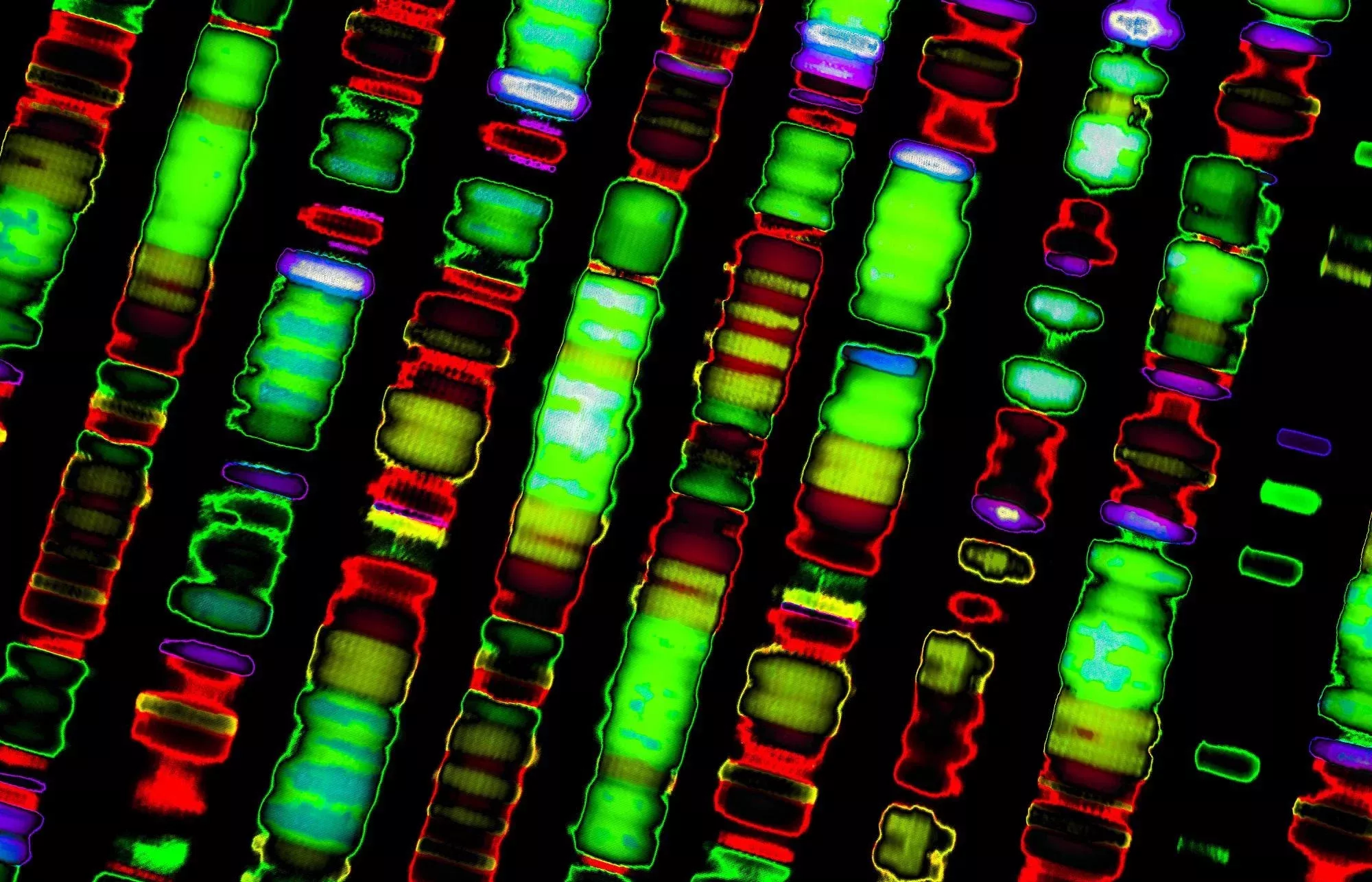
We ourselves have used a Seeplex® STD6 ACE Detection kit in a study on 224 Romanian subjects including persons with STD symptoms and asymptomatic individuals involved in unprotected sex with multiple partners, couples experiencing unexplained infertility or others requesting STD screening for various reasons. Each individual contributed with 30–50 mL FVU samples and DNA extraction was accomplished with MasterPure™ Complete DNA and RNA Purification Kits (Epicentre Biotechnologies, USA). A 2% agarose gel containing ethidium bromide was used with 0.5× Tris‐borate 0.1 mM EDTA (TBE) as running buffer. The PCR products were visualized using a UV transilluminator. An example of gel electrophoresis results can be visualized in Figure 1.

Figure 1.
STD pathogens—agarose gel electrophoresis. NC: negative control, 177–186: samples, PC: positive control, MK: marker, TV: T. vaginalis, MH: M. hominis, MG: M. genitalium, CT: C. trachomatis, NG: N. gonorrhoeae, UU: U. Urealyticum.
The accuracy of the method was demonstrated by the lack of contamination (no amplicons in the negative control band) and the presence of positive control bands corresponding to all six DNA fragments of known molecular weight included in the marker used to determine the size of the amplification products. Also, internal controls indicated proper PCR amplification in each microtube (see Figure 1).
About 74 (33.03%) of the 224 subjects, both symptomatic and asymptomatic, were positive for one or more STDs. All six pathogen agents were detected with the multiplex PCR kit, several double or triple infections demonstrating associative patterns. The following double associations were detected in the study: C. trachomatis and N. gonorrhoeae, C. trachomatis and U. urealyticum, N. gonorrhoeae and U. urealyticum, C. trachomatis and M. hominis. Several triple infections grouped C. trachomatis, N. gonorrhoeae and U. urealyticum.
The bacteria most frequently identified in the analyzed urine samples was C. trachomatis, found in 20.9% of the cases. Consequently, a number of associations between C. trachomatis and other STD agents (N. gonorrhoeae, U. urealyticum and M. hominis, respectively) were found. These results are consistent with studies conducted in other countries or international statistics indicating C. trachomatis as the most common STD agent [4, 52, 53]. Detection of C. trachomatis in several asymptomatic patients demonstrated again how easily this infection can pass unnoticed.
Some studies recommended that all sexually active women should be tested, pregnant ones or those that have experienced miscarriages in particular, given the high prevalence of C. trachomatis/N. gonorrhoeae infections [54, 55]. In the US, concomitant empiric treatment of C. trachomatis and N. gonorrhoeae is recommended for all gonorrhea positives considering the frequent association between the two pathogens [56]. However, results indicate that several other associations (such as those between C. trachomatis and U. urealyticum or M. hominis) are often encountered, suggesting that a population screening for C. trachomatis/N. gonorrhoeae is not good enough and a multiplex method for the simultaneous detection of the most frequent six or more STD agents would be more appropriate, considering the different associations that may arise.
N. gonorrhoeae was detected in 7.1% of the cases, as was the case of U. urealyticum. These results are consistent with other studies indicating a high prevalence of both bacteria, the most frequent STD agents except for C. trachomatis [9, 57]. A notable finding is that we detected patients positive to N. gonorrhoeae that presented no or very atypical symptoms of gonococcal infection, which could have resulted in inadequate treatment without this DNA‐based analysis that allowed us to identify the presence of the gonococcus. The N. gonorrhoeae/U. urealyticum coinfection we found was another confirmation that both C. trachomatis and N. gonorrhoeae can associate with other STD pathogens, an additional argument for the use of multiplex kits able to detect a large number of STDs in the same sample.
A recent study in Korea [58] found a 3.3% infection rate for T. vaginalis in the general population and argued that the rate was higher in women over 50 years of age. This followed a previous study documenting a 2.4% infection rate for T. vaginalis in the same area 15 years before and the significant increase lead researchers to recommend PCR‐based testing of T. vaginalis in all women over 50 years old, irrespective of their symptomatology. Our study detected but one (0.44%) case of T. vaginalis infection, suggesting that in our area prevalence is much lower than the literature data based on other than NAAT determinations (e.g., physical and microscopy examinations or cell cultures) indicated. NAAT seems to be for now the only accurate method to diagnose this parasite. Our results are consistent with those conducted in other countries where T. vaginalis was detected in similarly low percentages compared to other STD [43, 51]. However, the incidence of trichomonosis has gradually decreased over the past 40 years. This may be due to the large amount of metronidazole and other imidazoles generally used in the treatment of bacterial vaginosis. Although the number of people infected with T. vaginalis is low, the analysis is justified considering its asymptomatic manifestation and the serious complications it produces.
In a study conducted in the United States, M. hominis and various Ureaplasma species were detected in 21–53% of the cases involving asymptomatic women and 40–80% of the sexually active women, respectively, their prevalence being slightly lower in men [59]. In our study, mycoplasma infections were detected in 25 individuals (a rate of 11.1%), the most commonly encountered being U. urealyticum (in 7.1% of the patients). Although M. hominis and M. genitalium were less represented (1.7 and 2.2% of the patients, respectively), these infections cannot be ignored. More so considering that M. genitalium was detected in an asymptomatic patient previously found negative for different STDs investigated on specific culture media (including ones for M. genitalium) in a number of different specimens (urine, urethral discharge). This last example reaffirmed the sensitivity of the multiplex PCR method over traditional alternatives.
Add us on Line and stay in touch.
5. Advantages of the multiplex PCR method
The advantages of the multiplex PCR method were assessed by various researchers comparing the diagnosis results obtained with different other conventional methods. The sensitivity and specificity of these methods were analyzed on different specimens in comparison to traditional methods, some of these considered to be the gold standard in diagnosis [36, 43, 46, 51]. Although this method can sometimes increase the workload, implying more protocol steps (DNA extraction, purification—if necessary, PCR amplification, electrophoresis), it still holds a huge advantage in terms of the exact diagnosis of STD. Except for special circumstances, such as when testing susceptibility to antibiotics of the various bacterial agents, NATTs have become the most sought after tests in STD detection. Regarding bacterial resistance to antibiotics, the DNA extracted and identified as belonging to such bacteria may be genetically tested to determine the genes that induce resistance to antibiotics or the different mutations that cause such resistance.
Although the symptoms are often similar, the treatment may differ depending on the STD agent detected. Without an accurate diagnosis, treatment is often ineffective. Clinicians often employ point‐of‐care (POC) tests to diagnose vaginal infections and STDs. For example, most clinicians rely on Amsel's clinical criteria in defining bacterial vaginosis: increased vaginal pH, the presence of amines, clue cells observed on wet mounts and homogeneous vaginal secretions [60]. Although bacterial cultures and other methods are still widely used in STD detection, PCR tests are relevant, reproducible, sensitive and specific enough tools implying low costs and simplicity. In addition, the availability of commercial NAATs that include several STD pathogens allows more detailed studies regarding the relationship between such organisms in the etiology of these diseases. As well documented, all STDs occur in populations at high risk for other sexually transmitted infections. Their presence in a given individual is a marker for high‐risk behaviors and coincidental infections should be sought after, as well as other more serious sexually transmitted diseases such as HIV.
An advantage of this method is its great sensitivity consisting in the detection of STD pathogens in individuals who have previously been tested with conventional methods and came out with negative results.
The greatest advantage of this method is the detection of double or multiple coinfections. This is an important argument for promoting multiplex testing in the same sample. These results could have important implications in epidemiology and treatment by improvements in the accuracy of determining the possible synergies and interactions between such microorganisms.
STD screening for certain categories of population (e.g., patients attending sexual health clinics, infertile persons or women who had miscarriages) is necessary not only to identify symptomatic persons in order to diagnose and treat their infection but also to identify asymptomatic individuals who serve as possible infection carriers in order to reduce morbidity and help controlling these STDs. The multiplex PCR method provides a good opportunity to argue for STD screening.
Pricelist
| PCR for 14 Infections (STD Multiplex) | Online results | |||
| Same day | Next day | 3 days | 7 days | |
| Throat | 7200.- | 6990.- | 4500.- | 4200.- |
| Urine | 7200.- | 6990.- | 4500.- | 4200.- |
| Anal Swab | 7200.- | 6990.- | 4500.- | 4200.- |
| Vaginal Swab | 7200.- | 6990.- | 4500.- | 4200.- |
| Cervical Swab | 7200.- | 6990.- | 4500.- | 4200.- |
| Sperm | 7890.- | 7250.- | 5490.- | 5050.- |
| Skin Lesion Swab | 7200.- | 6990.- | 4500.- | 4200.- |
| Pooled Swab | 9400.- | 8600.- | 8290.- | 7750.- |
| PCR for 2 Infections (Gonorrhea/Chlamydia) | Same day | Next day | 3 days | 7 days |
| Throat | 5690.- | 4990.- | 3990.- | 3300.- |
| Urine | 5690.- | 4990.- | 3990.- | 3300.- |
| Vaginal and Cervical Swab | 5690.- | 4990.- | 3990.- | 3300.- |
| Rectal Swab | 5690.- | 4990.- | 3990.- | 3300.- |
| Skin lesion Swab | 5690.- | 4990.- | 3990.- | 3300.- |
| Sperm | 6200.- | 5150.- | 4100.- | 3690.- |
| Pooled Swab | 6990.- | 6400.- | 5790.- | 4590.- |
- *In case of repeat +3 days
- **Do test before 1 p.m.
- Prices are in Thai Baht
- Price per one location of testing
- Online results will be available at PULSE Online Portal (POP) and E-Doc mobile application
Trust PULSE CLINIC to take care of your health like other 45000 people from over 130 countries. We provide discreet professional service with high privacy. Here to help, not to judge.