Non-Sexually Transmitted Diseases Causes of Penile Discharge
23964
Penile discharge is a condition in which fluid collects in the urethra as a result of an infection.

Written by Dude Arnel Flores Lopez, BSN, RN 05 June 2021
Medically reviewed by Dr.Deyn Natthakhet Yaemim (Founding Director) 06 June 2021, Last updated 06 June 2021
Non-Sexually Transmitted Diseases Causes of Penile Discharge
Male discharge that has a non-STD cause may be a variation of normal discharge, or it could be a sign of an infection that requires treatment. The urethra is the tube through which urine and semen pass from the body. It can appear watery and transparent or opaque and cloudy containing pus and occasionally even blood. The odor may be unpleasant or not noticeable at all. It is easy to understand why this condition is so confusing for the average person considering the difference in the appearance of the discharge. Penile discharge is one of many signs of a more significant problem and should always be evaluated by a physician.

Causes of Penile Discharge
Several conditions can cause penile discharge. Urinary Tract or yeast infections are often the underlying factor and can be accompanied by pain or a burning sensation during urination as well as the need for frequent urination. These types of infections are generally easy to treat and with the proper medications, curable. Unfortunately, several STDs can result in this unwanted condition. The type of STD will determine treatment, but if caught early, almost all can be treated as well.
Signs and Symptoms

Burning and pain when urinating are classic symptoms of urethritis. You may also feel the urge to urinate more often than normal. Other symptoms can include itching, tenderness, or swelling in the penis, pain with sexual intercourse, or blood in the urine or semen. Some infections may also be associated with discharge from the penis. Painful ulcers on the genitals can be present with herpes urethritis, another sexually transmitted disease. Simple urethritis does not cause fever or severe illness. If the disease spreads to other organs in the genital or urinary tract or into the bloodstream, however, it may result in the following:
- Back pain
- Abdominal pain
- High fevers
- Nausea
- Vomiting
- Swollen joints and other symptoms of disease throughout the body
Non-STD Causes of Penile Discharge
A. Urinary Tract Infections
Most urinary tract infections (UTIs) are caused by the bacterium Escherichia coli (E. coli) which is naturally present in our bodies. An infection occurs when the bacterium enters the urinary tract through the urethra.
Other factors that increase your risk for UTIs in Men
- Diabetes
- Being uncircumcised
- Fecal incontinence
- Immobility
- Dehydration or not drinking enough fluids
- Engaging in anal intercourse exposes the urethra to more bacteria
If you are diagnosed with a urinary tract infection, it is necessary to drink plenty of fluids to increase urination levels. Urination will help flush the bacteria from your system. Antibiotics should be prescribed as well. It is always a good practice to take all the medications that your doctor prescribes. Discontinuing an antibiotic early encourages the growth of antibiotic-resistant bacteria. Occasionally, people will recommend drinking cranberry juice to eliminate a UTI or to speed up the recovery.
While there have been promising experiments with mice that suggested cranberry juice is helpful, this method is unproven. Penile discharge is only one of the symptoms that can be present with a UTI. Others can include burning during urination, lower back pain, and the frequent urge to go to the bathroom. If any of these symptoms are present, consultation with a physician is recommended.
B. Prostatitis
The prostate is a walnut-shaped gland that surrounds the urethra. It’s responsible for making prostatic fluid, a component of semen. Prostatitis refers to inflammation of this gland. The inflammation may be the result of an infection or injury to the prostate. In other cases, there’s no clear cause.
Possible symptoms of prostatitis include discharge and:
- pain
- foul-smelling urine
- blood in the urine
- difficulty urinating
- a weak or interrupted urine stream
- pain when ejaculating
- difficulty ejaculating
In some cases, prostatitis resolves on its own or with treatment within a few days or weeks. This type of prostatitis is known as acute prostatitis. But chronic prostatitis sticks around for at least three months and often doesn’t go away with treatment. Treatment may help relieve symptoms, though.
C. Smegma
Smegma is a buildup of a thick, white substance under the foreskin of an uncircumcised penis. It’s made up of skin cells, oils, and fluids. Smegma isn’t discharged, but it looks very similar. All of the fluids and components of smegma naturally occur in your body. They help keep the area hydrated and lubricated. But if you don’t regularly wash your genital region, it can start to build up and cause discomfort. Smegma also helps create a moist, warm environment. This can increase your risk for a fungal or bacterial infection.
D. Balanitis
Balanitis is inflammation of the foreskin. It tends to happen in people with uncircumcised penises. While it can be quite painful, it’s usually not serious.
In addition to discharge, balanitis can also cause:
- redness around the glans and under the foreskin
- tightening of the foreskin
- odor
- discomfort or itchiness
- pain in the genital area
Several things can cause balanitis, including:
- skin conditions, such as eczema
- fungal infections
- bacterial infections
- irritation from soaps and other products
Ruling out an STD
If you’ve ever had any type of sexual contact, it’s important to rule out an STD as a potential cause of your discharge. This can be done with simple urine and blood tests. Gonorrhea and chlamydia are two of the most common causes of penile discharge. They require treatment with prescription antibiotics. Keep in mind that STDs don’t just result from penetrative intercourse. You can contract an STD by receiving oral sex and engaging in nonintercourse activities. And some STDs don’t cause symptoms immediately. This means you could still have an STD, even if you haven’t had any sexual contact in months. Left untreated, STDs can cause long-term complications, so it’s important to treat them. This also reduces your risk of transmitting an infection to others.

ABC’S of Preventing Infection
A - Abstinence from any sexual contact (or skin-to-skin contact) is the only absolute way to prevent STIs.
B - Be faithful. Being in a long-term, monogamous relationship also is a good way to avoid them.
C - Condoms are the only type of contraception that can both prevent pregnancy and protect against sexually transmitted infections (STIs). There are 2 types of condoms:
- external condoms, worn on the penis – sometimes called male condoms
- female condoms, worn inside the vagina – sometimes called female condoms Condoms are made from very thin latex (rubber), polyisoprene, or polyurethane and are designed to stop your semen from coming into contact with your sexual partner.
D - Drug prophylaxis. PrEP (Pre-exposure Prophylaxis) is a prevention method used by people who are HIV-negative and at high risk for being exposed to HIV through sexual contact or injection drug use. When someone is exposed to HIV through sex or injection drug use, these medicines can work to keep the virus from establishing an infection.
PEP (Post-Exposure Prophylaxis) refers to the use of antiretroviral drugs for people who are HIV-negative after a single high-risk exposure to stop HIV infection. PEP must be started as soon as possible to be effective always within 72 hours of possible exposure – and continued for 4 weeks.
E -Education to build on the knowledge, skills, and behaviors, thus enabling young people to make responsible and safe choices. Good sexuality education focuses on love, safer sex, abstinence, respect for others and oneself, diversity, personal rights and responsibilities, relationships and friendships, effective communication, decision-making, and risk behaviors.
Where can I test and get the treatment of Non-STD penile discharges?
Contact us at info.bkk@pulse-clinic.com or chat on your preferred platform:
Add us on Line and stay in touch.
Diagnosis
non-sexually transmitted causes of penile discharge, such as balanitis, non-gonococcal urethritis, prostatitis, and urinary tract infections, are important to consider when evaluating this symptom. These conditions may stem from bacterial, fungal, or inflammatory origins often related to hygiene, irritants, or systemic infections. Diagnosis generally involves a physical examination, urinalysis, and in some cases, culture tests or polymerase chain reaction (PCR) tests to accurately identify the cause.
PCR 28, particularly a 28-day post-exposure PCR test, can be highly useful in detecting low levels of bacterial or viral DNA that traditional methods might miss. This sensitive testing method aids in rapid and accurate diagnosis, allowing for early, targeted treatment that includes antibiotics, antifungal medications, and improved hygiene practices. Swift identification and intervention help prevent complications and ensure effective symptom relief.
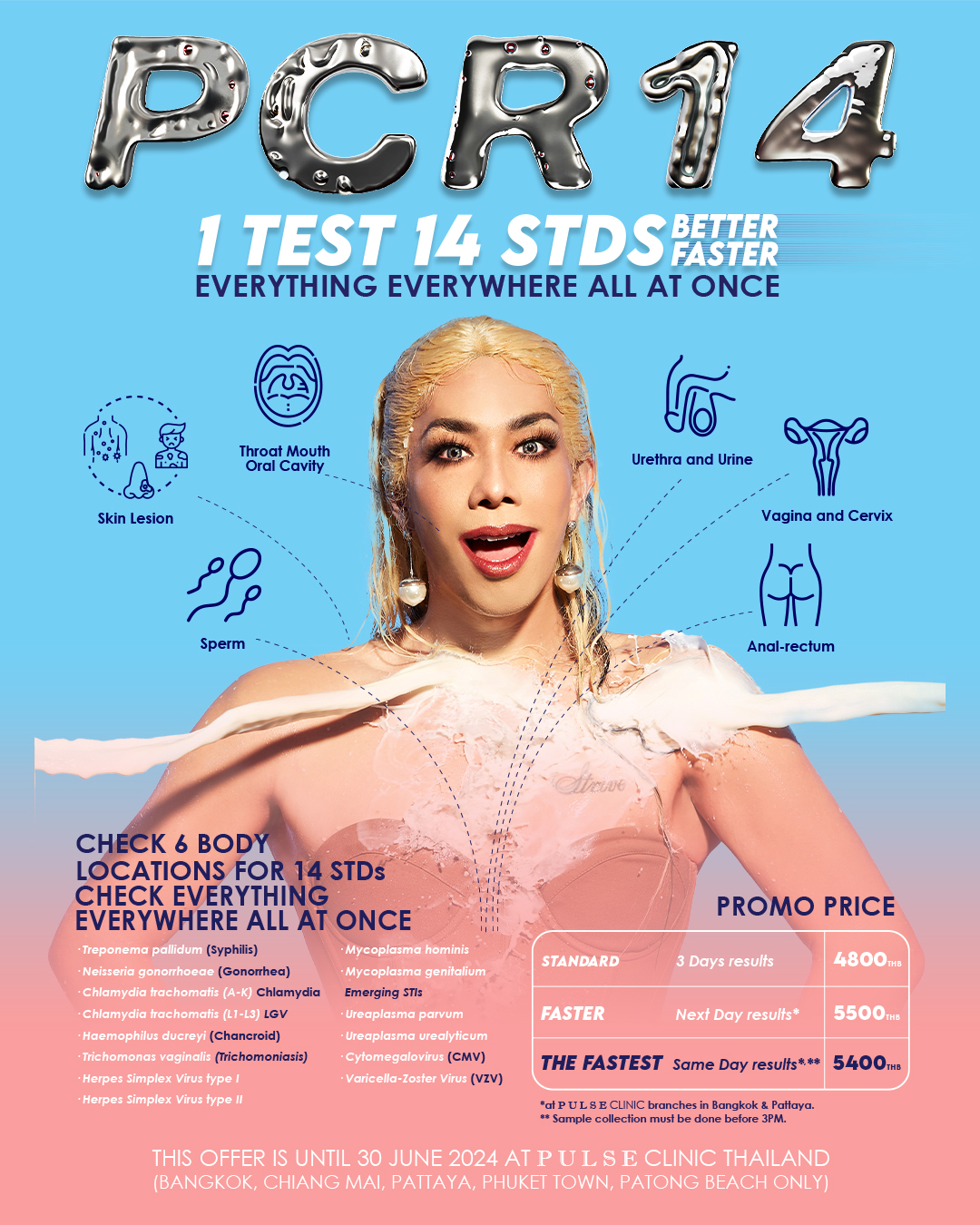
PCR 28 for Sexually Transmitted Diseases (STDs)
PCR 28 can provide comprehensive testing for 28 pathogens related to STDs and other related symptoms. PCR stands for Polymerase Chain Reaction; it is also called Nucleic Acid Amplification Test (NAAT). It is a modern molecular technique used to detect a particular pathogen (virus or bacterium) in a specimen of blood, body fluid, or other tissue. This technique detects virus or bacterial DNA. The nucleic acid amplification test (NAAT) is the recommended testing method for Chlamydia, Gonorrhoea, Ureaplasma, Mycoplasma, and Trichomonas, among other infections. It has higher specificity (higher than 99.5%) and higher sensitivity and accuracy than culture (the old diagnosis technique). In both men and women, painless urine PCR (yes, you just have to pee) and genital PCR were significantly more sensitive than culture. It can detect infection, whether the organism is dead or alive! This is mostly done in first-world countries and medical schools.
All PULSE clinics in Thailand provide the most comprehensive PCR tests for 28 infections to give you peace of mind and fast treatment.
Book your PCR Test today!!
Contact us at info.bkk@pulse-clinic.com or chat on your preferred platform:
Add us on Line and stay in touch.
Loading...
Clinic Locations
Loading...